How useful are CGMs for athletes?
Literally noone asked for this much info but here you go
As I noted in this post, I see quite a few athletes in my practice who've got elevated blood glucose. Initially, these were nearly exclusively patients who had been found to have an elevated HbA1c at a regular doctor's visit. Increasingly - and probably influenced by the fact I write a lot about CGM's - I see patients in my practice who use CGMs, see some weird glucose rises and have questions.
The aim of this post is to equip people with the knowledge to counter stuff like the AGGRESSIVE marketing from the guys at S*************s:
I will:
cover what athletes should expect to see when they use a CGM
be a bit of a debbie downer on the technological limitations of CGMs
discuss the potential usefulness of CGMs and how I think these devices can or could be valuable in the future
emphasise that CGMs will only ever be an adjunct to sports nutrition and why
I spent my last post whinging about people cosplaying expertise, so I want to be very explicit and emphasise I don't do any active research in this area. I am not an exercise physiologist. The below folks are some of the true experts who do/have done some phenomenal studies on glucose homeostasis in exercise/for athletes:

What athletes might see when they use a CGM
Disclaimer: the effect of exercise on glucose will be affected by prior exercise and previous food intake (which influence glycogen stores amongst other things), plus type of activity, length of activity and training status of the individual. Most studies have protocols which are not comparing like for like so definitive guidance is hard to come by. By this should help:
Second disclaimer: from my own clinical experience and from the literature, CGMs are predominantly used by endurance athletes - so I will focus on this in this post.
Glucose commonly increases in the immediate post-exercise period:
Glucose can significantly increase in the period immediately following intense or prolonged aerobic exercise (most studies have measured this starting about 30 mins after exercise finishes).
It occurs even in the absence of food intake and the glucose tolerance means that a person will have an exaggerated response to any carbohydrate they consume in the immediate post-exercise period.
Note that this is a phenomenon that seems to occur in most people if the exercise session is demanding enough, trained or not.
Glucose can significantly increase during super intense exercise:
Glucose can rise a lot during intense exercise - in the order of 2mmol/L (36mg/dL). This fascinating study examined this during HIIT in trained endurance athletes (see graph below). There seems to be a question about whether this can occur or not in untrained individuals. The magnitude of effect in untrained individuals looks lower, eg in this study, especially if you compare it to the obvious increase in glucose in type 1 diabetes.
It does not occur in prolonged but not too demanding aerobic exercise (see below).
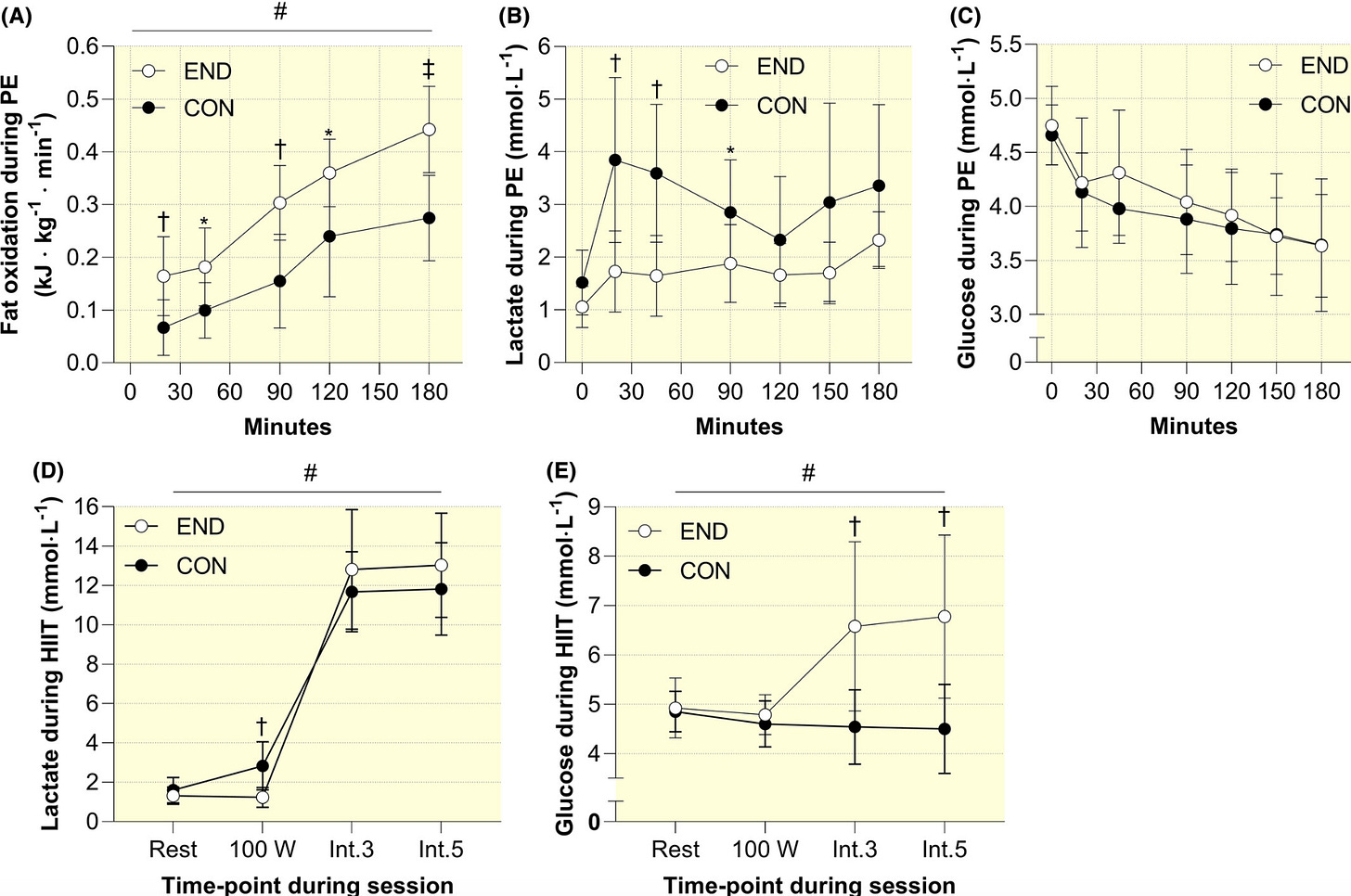
Glucose intolerance occurs the morning after prolonged exercise in trained individuals
The common assumption about exercise and glucose tolerance is that - once the immediate post-exercise period is over - glucose tolerance improves the following day and lasts a few days. So it’s interesting that it might worsen the day after in trained endurance athletes. The authors of the study shown in the figure below suggest this effect only occurs in trained endurance athletes and not controls. It looks to me as though something is happening in the controls (a lot of variability in glucose here though which is to be expected), and the literature is mixed as to whether this can occur in untrained individuals.
I should emphasise that defining the time course of changes in glucose after exercise is challenging because ideally you want to continually measure it for days from the moment a person finished exercise! You’d have to [Prior to CGMs woo!!!] take blood samples every hour after an exercise bout and keep doing that for at least 48 hours, and then make sure all meals etc were controlled. This study tested glucose tolerance every morning with an OGTT in moderately trained individuals and found improved glucose tolerance the day after 45 mins of cycling but they tested after a few weeks of intense exercise, not just an acute exercise bout. (See what I mean about being hard to draw conclusions because protocols are different?)

A small proportion of endurance athletes might have glucose profiles that look “prediabetic”
I used to think that this type of prediabetes in athletes was commonly characterised by an elevated fasting glucose, but normal post-prandial. This was because of anecdotal data from my own clinic and small studies in the literature. However, other new data show different. I think it’s safe to say this is a group which is not well characterised. Regardless of the presentation of “prediabetes” - in the absence of any well-defined clinical risk factors for type 2 diabetes (eg, family history, abdominal obesity etc) - I doubt these individuals are at risk of developing type 2 diabetes.
It might be reasonable to assume that in people who are performing frequent, demanding bouts of activity, that once you take into account 1) their during vigorous activity hyperglycaemia, 2) immediate post-exercise hyperglycaemia, and 3) delayed post-exercise hyperglycaemia - then effectively glucose is elevated frequently enough to push up HbA1c. It would be interesting to see what happens to endurance athletes if they take two weeks off any intense exercise to see whether glucose returns to normal…..
MEASUREMENT LIMITATIONS OF CGMS
In addition to being aware of the crazy glucose changes that can occur before and after exercise, the other major point I want to get across for athletes using CGMs is their ..in..accuracy.
CGMs have well-documented general limitations - for example, they give different readings based on body placement (sensor on leg produces lower values compared to arm at rest), whether it’s placed on the right or left arm and the devise used for example. Also, there is so much variability (noise) from these devices that some of the findings of differences in glucose readings from these studies might also just be noise haha.
But for athletes, the important thing to know is that sensor glucose can be particularly inaccurate during exercise. Accuracy of CGM sensors is affected by things like tissue pH, oxygen concentration, and skin temperature. Depending on the exercise, or whether carbohydrate is consumed, and where the sensor is placed, a CGM might over or underestimate blood glucose. This is a significant limitation when we consider relying on CGM data to assess fuel needs.
CGM sensors measure interstitial glucose (reflecting the local environment around the cells in which glucose concentration changes slowly) not arterial or venous glucose (the transport system in which concentrations of glucose change rapidly) - and this can produce a discrepancy between sensor glucose and “blood glucose” at times of rapid glucose change.
I present this case study just because the way they present the data is really clear - you can see the degree to which sensor glucose underestimates actual blood glucose during the cycling day when snacks were taken. Again - imagine relying only on the CGM to tell you about carbohydrate availability:

There’s a lot of work being done - and still to do - to assess and understand the accuracy of sensors for athletes with and without diabetes.
All of this is not to say CGMs are useless. It’s just that data you get from them should be interpreted with caution and with knowledge of when and in what ways they could be giving you inaccurate info.

The potential usefulness of CGMs!!
Now we get onto the good bit! I think the following are areas where these devices can or could be useful. We don’t have any good studies or data on this yet so this is all a bit theoretical.
Ensuring sufficient carb availability by making sure glucose concentration doesn’t decline during exercise.
Prolonged moderate/vigorous endurance activity depletes liver and muscle glycogen. Sufficient carbohydrate during exercise can prevent the decline in liver glycogen, and afterwards ensures repletion of muscle and liver glycogen. While sports nutrition guidelines offer target ranges of carb intake - eg 7-10g/kg - sensor glucose during exercise could support an athlete in personalising intake to ensure they have sufficient carbohydrate availability* (whether endogenous or exogenous) to train optimally.
Ensuring sufficient/optimal re-fueling
Consuming enough carbohydrate in the post-exercise period is important to replenish glycogen stores. If sensor glucose declines overnight this could be an indication of insufficient intakes.
An example of how this type of insight could be useful came up in a session I did for UKSI last week. Insufficient fueling can manifest in low nocturnal glucose readings - the coaches in this case advised a bigger evening meal with more carbs. Nocturnal glycaemia increased and performance improved.
Ensuring sufficient calories
If people don’t get enough calories, their glucose will decline over days and weeks. This an extreme example but 7 days of 600kcal a day causes glucose to go from 9.2mmol/L to 5.9mmol/L in people with T2D. A reduction in overall glucose (fasting or overnight glucose may be a particularly helpful parameter) could alert an athlete or training team to insufficient energy intake before it’s obvious in changes in weight.
Allowing the athlete to alter dietary intake in different training environments
Athletes may have a dietary protocol that works for them - but the effectiveness of the protocol might be affected by a changing environment. An example of this is at altitude - where rate of gastric emptying reduces. Potentially by understanding what their glucose profile looks like under ideal conditions, they can attempt to match it by altering intake (eg more easily digestible carbohydrates) at altitude.

Looking to the future a bit:
In addition, by recording and collecting CGM data in physiological exercise studies alongside gold-standard measurements like glycogen content, CGM use could theoretically help guide dietary periodization/carb periodization/”train-low” training:
The goal of this type of training - which basically aims to train under conditions of low glycogen - is to enhance oxidative capacity (such as increased mitochondrial biogenesis, lipid oxidation capacity and angiogenesis.) One of the challenges of doing this in practice is that a lot of guesswork (and athlete-specific, training type, previous training etc) goes into aiming to get an athlete close to or within the glycogen threshold. Potentially - CGM use could held guide the manipulation of dietary intake/training schedules to achieve glycogen depletion.

CGMs are merely an adjunct to evidence-based sports nutrition!
I just want to emphasise these points (I am sure most people are aware of these) to remind everyone to stay away from taking a gluco- or CGM-centric approach to anything!
They measure circulating carbohydrate but can’t tell us about glycogen stores.
Ultimately, this is what is going to influence maintenance of optimal training intensity and performance.
They don’t tell us anything about adequate protein intake
In amateur endurance athletes I would say the single largest nutritional issue I see is inadequate protein intake. Protein is obviously essential for muscle protein synthesis and recovery but also (alongside getting sufficient carbohydrate) optimises glycogen storage.
CGMs obviously don’t tell us anything about getting sufficient protein. Moreover, adding in more protein (to reach requirements) can even lower post-prandial glucose - and this might worry the athlete that they’ve messed up their nutrition. The athlete is now fueling correctly, but their CGM tracer might indicate to them their carb intake is now too low…?
I included other things like oral carbohydrate sensing and lactate in my presentation to kind of labour the point about limitations of CGM but won’t do that here.
CHEERS!
Disclaimer
As a dietitian, and not a medical doctor, I am not qualified to diagnose any health conditions.




I wonder if HIIT being used in studies is throwing off a bit, most endurance athletes do a lot of long slow work/aerobic base building.
Thank you for this info and your review of this in Prac Diabetes.
I have seen healthy normal weight patients exclude foods believing they were pre-diabetic/ insulin resistant from a normal glucose spike. At least now I can reassure them!