One of the most intriguing population groups I see in my practice is athletes [or modest people who wouldn't describe themselves as athletes but they do such an extraordinary volume and intensity of exercise that they are basically athletes!] who have been told by their GP that they have prediabetes based on either a fasting glucose or HbA1c measure.

Prediabetes is an umbrella term for at least two separate conditions (impaired fasting glucose/impaired glucose tolerance) that describes blood glucose which is higher than normal but not high enough to meet the threshold for a diagnosis of type 2 diabetes (T2D). Prediabetes is the term generally used because it serves as a bit like an alarm bell that a person is at increased risk of T2D.
Although some non-modifiable factors increase a person’s risk of developing T2D, changes in our lifestyles are the largest contributor to the T2D epidemic. At least 80% of people with T2D have a BMI >25kg/m2, and physical activity is inversely related to T2D risk.
So, you can imagine the concern (and surprise!) that a very athletic person with a low BMI and low body fat percentage feels being told that they are at risk of a serious cardiometabolic disease.
And what's curious about these patients is that nearly all of them have no classical risk factors for T2D, eg: no family history of T2D, they have normal blood pressure, low body fat, their diets are generally pretty good and they also do a lot of physical activity.
So what is going on with these patients?
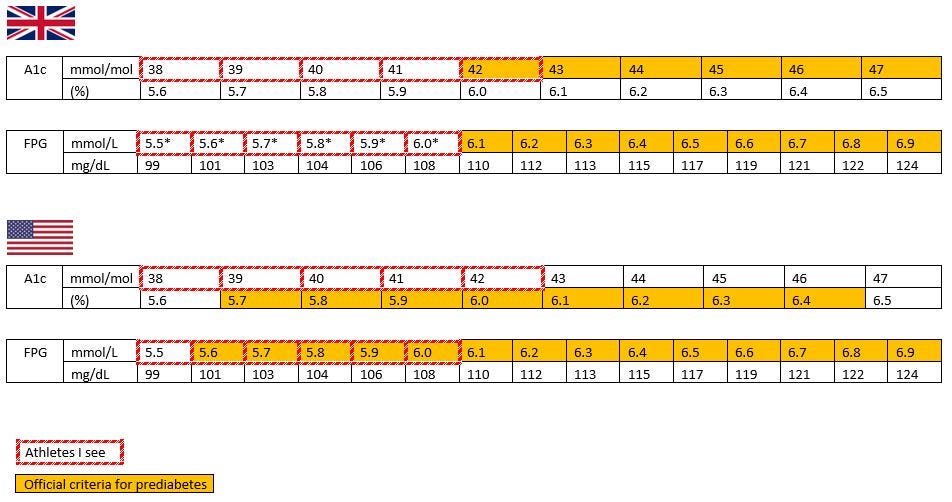
These athletes I am talking about will typically have an HbA1c of 38-42mmol/mol (5.6-6.0%). Or, they might have a fasting glucose of 5.5-6.0mmol/L (99-108mg/dL). (Yes, the lower cut-off for prediabetes in the UK is 42mmol/mol or a fasting glucose of 6.1mmol/L, but some GPs/practitioners might flag the glucose if it’s higher than they expected). The US has different criteria as shown below:
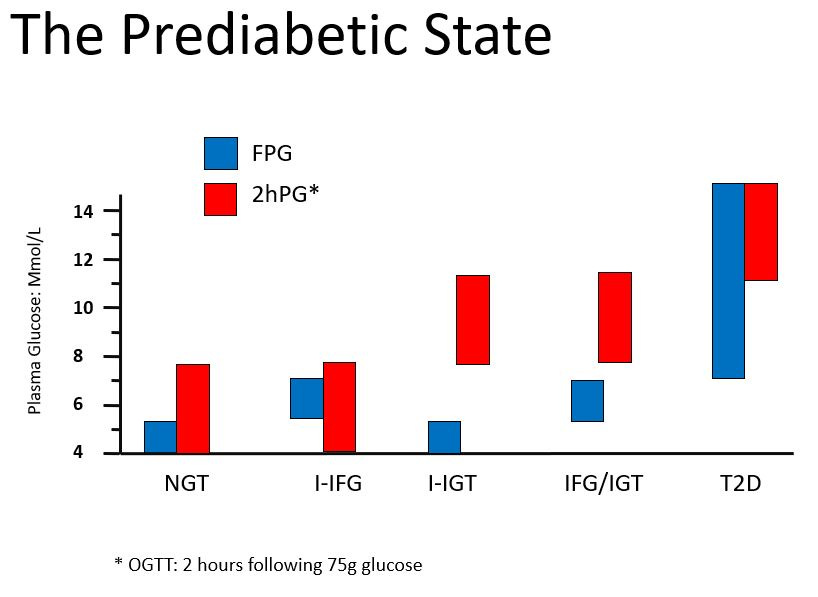
A high HbA1c can mean that a person’s fasting glucose is high OR their postprandial glucose is high OR both. In general people with just an elevated fasting glucose will have an HbA1c on the lower side of the “prediabetic” range while people with elevated fasting AND post-prandial glucose tend toward the higher HbA1c range.
And every single one of these athletes I see has a glucose which is elevated in the fasting state only.
If I test their response to an oral glucose tolerance test (OGTT) the fasting measure is elevated. But.. they are able to manage a 75g load of glucose very effectively such that their glucose lowers rapidly and is typically <5mmol/L (<90mg/dL) by 2 hours. (You can also get a reasonable indication of fasting vs post-prandial glucose from a continuous glucose monitor (CGM) readout).
As I said above, prediabetes is actually a bunch of different conditions:
Isolated-impaired fasting glucose (only fasting glucose is high)
Isolated-impaired glucose tolerance (only post-glucose load/post-prandial glucose is high)
Impaired fasting glucose and impaired glucose tolerance (fasting and post-glucose load/post-prandial glucose are high)
Isolated-impaired fasting glucose (I-IFG) and isolated-impaired glucose tolerance (I-IGT) have a distinct pathophysiology. In short, isolated-IFG is characterised by marked hepatic insulin resistance while muscle insulin sensitivity is pretty normal. Conversely, isolated-IGT is characterised by marked muscle insulin sensitivity but minimal hepatic insulin resistance. (There are also some differences in beta-cell function).

So what's going on with these athletic patients?
There isn’t a ton of literature that I could find. This small study using CGMs found that fasting glucose was in the ADA prediabetes range for 3 out of the 10 young, lean endurance athletes. I also reached out to a fantastic physiologist - Dr Javier Gonzalez at the University of Bath to ask him about this. His research specialises in physical activity and carbohydrate metabolism, and he does a lot of work with athletes. His preliminary data do suggest that objectively measured physical activity energy expenditure (PAEE) is positively related to mildly elevated fasting glucose.
A commonly-heard explanation is that glucose might run high due to high cortisol but I don’t see elevated cortisol in these patients, and in any case the relationship between endurance training and cortisol is not consistent or straightforward anyway. And by the way, all the fasting insulin measures I have seen in these patients are in the normal range too.
It actually looks like athletes have lower fasting insulin secretion than controls
Several old-school studies have shown that athletes have lower fasting insulin secretion, and a fasting insulin concentration 50% lower than controls. This very cool study shows the frequency of insulin pulses between athletes and controls is the same, but the amount of insulin secreted during each pulse is lower in athletes.
But this doesn’t explain the observation that fasting glucose seems to run higher than the normal physiological concentration in some athletes. In normal glucose metabolism, the body keeps fasting glucose in a pretty tight range. According to common understanding (at least mine, ha ha) we would expect that any rise in glucose above ~5.5mmol/L would cause the pancreas to release just enough insulin to bring glucose down again.
Dr Gonzalez speculated whether there was higher glycolytic flux in these patients, which might be a naturally-occurring physiological adaptation to endurance exercise. There is a definite need for some cool isotope studies in this population to track where glucose is coming from and going to, and how the beta-cells are responding. And also why it only seems to occur in some athletes….
I’m an athlete, with slightly high blood glucose - do I need to be concerned?
The most precise way of determining individual risk of T2D is by using some validated risk calculators"*:
American Diabetes Association Risk Test
As I mentioned, most of the athletes I see have zero risk factors for T2D apart from mildly elevated fasting glucose. So they’ll find their risk using these calculators is low. We cannot say with absolute certainty that these individuals will not develop T2D in the near future but the risk is very, very low. It’s always smart to get an annual HbA1c or other glucose check to keep an eye on things, but otherwise my advice is to relax.

Others question whether a fasting glucose value which is slightly but chronically elevated causes other health concerns. This is really difficult to answer because we simply don’t have good data on it. For example, there are Mendelian randomisation studies which suggest modestly elevated glucose is associated with things like arterial stiffness. But, these studies didn’t look at post-prandial glucose excursions. So we can’t know for sure that this is due to fasting and not post-prandial excursions. For the average person with an elevated fasting glucose, it’s likely that their post-prandial glucose is also elevated to the same degree because baseline glucose is higher.
But we are not dealing with an average population - athletes are exquisitely insulin sensitive and are better at disposing of glucose via insulin-independent mechanisms too. So, unsurprisingly, they are able to dispose of a massive amount of carbohydrate very, very quickly and need much less insulin to dispose of the same concentration of glucose compared to controls. There is really fascinating data suggesting there are adaptations in the beta-cell in athletes which cause it to produce less insulin in response to multiple insulin secretagogues. It’s almost like in trained athletes the body is saying “yeah, we can dispose of glucose so efficiently we’re not going to need much insulin”. So athletes are very likely to have normal post-prandial glucose, even if their fasting might run slightly high.

So overall, my advice to any athlete concerned about moderately increased fasting glucose in isolation is that it’s probably nothing to worry about. (And no, I wouldn’t even worry about fructose but we’ll cover that in another post!).
(*Although these calculators might seem really boring and basic, adding in genotyping at best only slightly improves their predictive value).



Excellent article. I’m an athlete and the phenomenon I am dealing with is normal fasting glucose(85) , low insulin (2.5), but high A1C (6.2). I’ve searched high and low to understand this and doctor says “I’m fine”…. Would love help in understanding why markers don’t always align.l and how this makes sense.
Thank you. Well written and researched.
I look at Type 2 Diabetes as not a “sugar” problem but actually a chronic excess storage problem.
In reality glucose is the last “marker” to rise in a true type 2 diabetic. They have many other markers rise before glucose including fasting insulin, triglycerides, Leptin and organ markers (liver function tests). They also have decreasing Adiponectin over time.
So fasting glucose is a not so great marker to diagnose diabetes.
I still want a better explanation though of A1C rise in people without diabetes. Just healthier rbcs isn’t enough of an explanation.