In my clinic, I’ve seen quite a few endurance athletes (without diabetes) using continuous glucose monitors (CGMs) who have really spiky readings—big jumps and drops in their blood sugar levels. They don’t always feel any different when these spikes happen, but it still raises concerns when they see those numbers all over the place.
After looking into their diets, I noticed a common theme: they weren’t getting enough protein. Once we increased their protein to around 1.2 to 1.5 grams per kilogram of body weight—depending on their training and activity level—their CGM readings started to smooth out.
These are my musings on what this might mean (as a non-exercise physiologist, and more of an interested by-stander):

What’s going on?
Much of the research on and interest in protein requirements has centered around strength training. Of course this makes sense because muscles are made of protein, and if you want to grow bigger and stronger muscles… it seems obvious you need more protein. And when I see strength training folks in my practice, they’re pretty spot on in hitting their protein targets.
But what about people who primarily do high intensity and often long lasting aerobic exercise? I see folks who are on the bike for 60+ mins a day, pedalling at what they describe as “full pelt” throughout.
It’s fair to say that there is a lot of debate around how much protein exercisers - both strength and endurance folks - need. But it is acknowledged in the field that the method used to determine protein needs for the wider population (nitrogen balance) is not sufficient to determine how much protein intense exercisers/athletes need for optimal performance and recovery for several reasons: it tends to overestimate how much nitrogen people retain at higher protein intakes; it does not take into account the elevated amino acid oxidation which occurs during exercise; and it tells us nothing about what is extremely/most important to keen exercisers/athletes: performance.
It also seems methodologically a bit trickier with endurance athletes because beneficial training adaptations to aerobic exercise include an increase in the size and density of mitochondria, but mitochondrial protein synthesis is not captured from muscle protein synthesis (MPS) which is what most studies measure.
But there does seem to be a consensus that endurance athletes need more protein. The American College of Sports Medicine (ACSM) recommends 1.2–1.7 g/kg for endurance athletes or people “training for a cycling or running event”.
But how do you know if you’re an endurance athlete? And many people work-out hardcore without actually training with a specific event in mind…
So if you’re an exercise-at-full-pelt cyclist/rower or longer-than-average distance swimmer/runner, how do you know if you should be getting more protein?
I had a lady come to see me who was unsure of how much protein she should have because she’d head from some podcast or blog that unless people were elite athletes or spending “8 hours a day" exercising that there is not requirement for extra protein. This is incorrect.
And this perspective of “I am not Eliud Kipchoge, therefore I am regular person with regular nutritional needs” is quite widespread in intense aerobic exercisers from my experience.
I've seen “regular” folks who do an hour of rowing in the am and 1 hour of weight training in the pm three times a week, plus a long ride on a Sunday, plus additional zone 2 or high intensity training on other days of the week. “Regular” folks who do 60 to 90 minutes of cycling at an intensity where they find it “difficult” to speak. And of course I’ve seen people training for half or full marathons, and taking it SERIOUS. And these people tend to be pretty modest people with full-time jobs who just consider themselves normal people trying to stay very physically fit.
Knowing at what level protein requirements start to increase is not helped by the research on endurance/vigorous aerobic exercise and protein metabolism having different exercise protocols in terms of duration or intensity. And some studies have included trained and some untrained individuals (which matters because protein utilisation seems to adapt to exercise over time).
So we lack the specificity to be able to say “well if you’re doing more than X mins, at X intensity then you’ll need more protein”.
And then there’s the issue of carbohydrate. Recommendations for carbohydrate do increase with aerobic activity, particularly longer than 60 minutes. And with very high level athletic training, there are marked improvements in performance with more vs less carbohydrate. But sadly, given the fear mongering about glucose spikes on CGMs widely - and of course from these patients’ perspectives they're already getting erratic glucose - you can understand any reluctance to consume glucose gels or pile on the rice. And of course, how much protein you need is influenced by how much carb (and calories) you're taking in.
One thing I have always asked people in my practice is “how do you feel? [after training/in the morning]”. And quite often, insufficient fueling generally - which of course includes protein - is associated with some kind of comment like “I feel a bit battered when I wake up”. I was a long distance runner during my 20s - and while I had the carbohydrate covered (massive pizzas, dates and bananas) - if I skimped on protein, I would feel a bit run over in the morning. So this can be a clue that you need to re-think your nutrition, including protein.
But then I have been seeing this erratic CGM stuff with the people whose protein remained around 0.8g/kg.
What does the spiky CGM read out look like?
A bit like this:
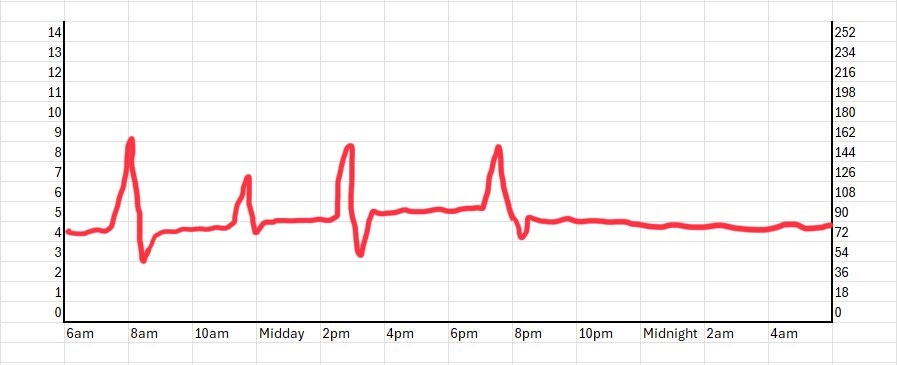
It's important to note that the glucose rises and falls that people seem to be getting are within what we understand to be normal limits (notwithstanding accuracy limitations of CGMs), but the erratic nature of these the glucose profiles is unusual. It's not like glucose is just going up following a vigorous bout of aerobic exercise as I described here. On first glance it looks like people have a bit of reactive hypoglycaemia, but these peaks and drops are not associated with any symptoms like dizziness or anything. And on questioning, these individuals didn't have a close family history of any kind of diabetes that they knew of.
And while rebound hypoglycemia can occur upon initiation of exercise in healthy people - this wasn’t what was going on in these individuals. The very rapid dips on the readout were in response to pretty much all meals. I also checked out this previous publication which had used CGM’s in athletes, and a few participants also seem to have very high, highs followed by very significant drops to their meals.
But this erratic glucose profile is counter-intuitive from a physiological perspective. Very aerobically fit people are incredibly insulin sensitive, so by extension I would think that if there is excess glucose in the blood it should be taken up by the muscles for oxidation during activity or for glycogen replenishment after activity.
So having glucose that goes up and down pretty much in response to every meal was something I was curious about.
More protein smoothed out the glucose excursions
However, unrelated to the glucose spikes, upon dietary review they weren't having enough protein, so naturally this is something I recommended people get more of. But lo and behold I've now seen four of these people since, and the additional protein seems to have smoothed out their glycaemic excursions.
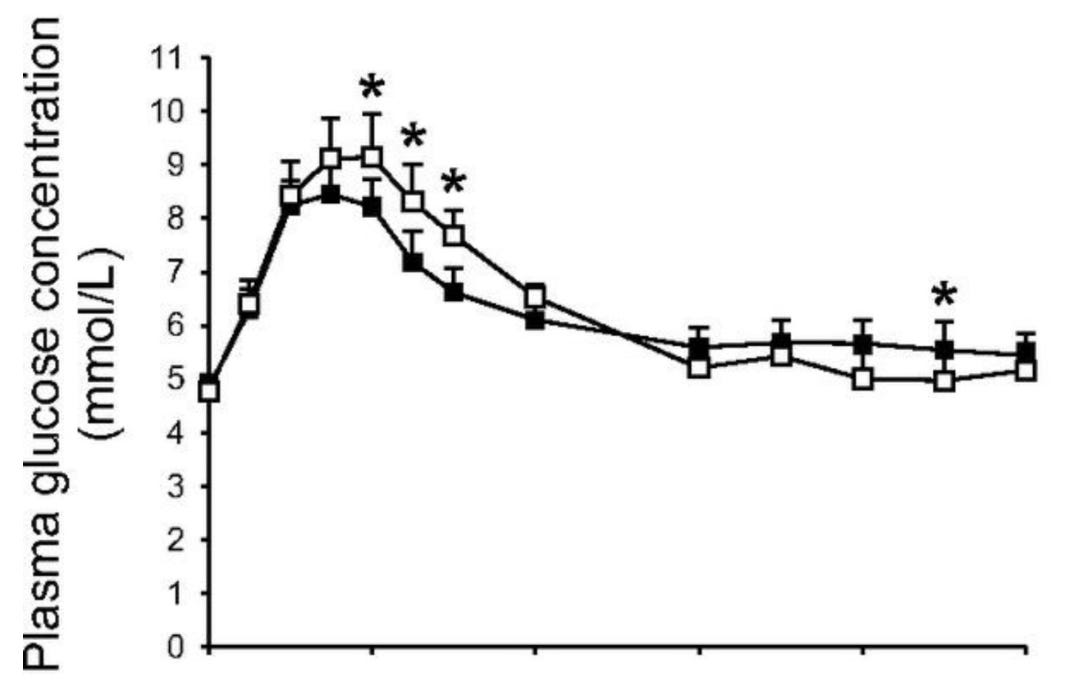
It does make sense to me that additional protein could lower the glucose peak after a meal, because we know protein is insulinogenic (makes the pancreas secrete more insulin). However, since protein is insulinogenic…. (!), you might think that the additional protein would cause an even more exaggerated fall in blood glucose. But this isn't what we see on the glucose read-outs.
My speculative musings as more of a beta-cell specialist as opposed to a whole body physiologist is that perhaps the lack of protein is somehow affecting the beta-cell machinery (which of course are all proteins) - this causes failure of the first phase insulin response (so you get the peak); and the second phase overshoots, (which causes the dip). Then maybe once people get more protein, their beta cell phasic responses work properly again? Who knows.
If you’re getting an erratic CGM and you do a lot of exercise should you consume more protein?
I think it’s too premature to suggest this yet. I recommended additional protein because based on my assessment it seemed to be the major nutritional piece lacking. The smoothing out (and by the way I am not saying smoother is necessarily better) was just a very interesting observation.
For example, do I know that this effect was due to the protein itself and not merely the fact that people were fueling more and the same might have been achieved by adding more carbohydrate or even fat in? No.
But perhaps if you're seeing weird erratic glucose profiles that you can't explain, maybe take a look at how you're fueling your activity and think about whether additional protein might be required.
At the end of the day the most important thing was that each of these individuals upon increasing their protein came back and said they felt much better and felt like they were recovering from exercise much better.
Finally I'd like to note how valuable it is for me to be able to see patients clinically. I am always fascinated by the patients I see, love listening to their stories and it's always a great way to learn and have to go back into a delve into the literature about things. And while exercise physiology isn't my area, I pass on lots of these observations to physiology boffins just in case they think they’re interesting or worthy of exploration. And where clinical observations are relevant to the research I do, I have been able to design trials to test things that seem to be important to patients. On that note, I am writing up this study currently, and hopefully it should be out in the new year! Cheers.







Thank you for these important clinical observations! In my experience protein is a key component in reducing reactive hypoglycemia. It has been postulated that this is due to protein not only being insulinogenic but also stimulates glucagon and thus helps the body ‘balance’ blood glucose levels. Could this be an additional effect that you are observing? Love to hear your thoughts!
Something to factor in with protein guidelines and high-volume endurance athletes is how much protein (and everything) they should be eating due to their total output
When I'm in-season, I'm training ~3 hours a day(avg). This past summer, I did a doubly labeled water study (Calorify) and that had my "burn" at 4000kcal per day.
https://feelthebyrn.substack.com/p/burn-part-three
At any reasonable split (Pro, Fat, Cho) I'll be well above standard guidelines for protein.
The numbers above are as a 55 yo male. When I was younger, and racing elite, my volume was higher and my intake was higher, too. Unfortunately we didn't have DLW studies back then but there have been a few done on modern high-volume elite triathletes.
Thanks for your writing - I find it interesting.
G