Reactive hypoglycaemia
Reactive hypoglycaemia whether clinically confirmed or suspected by the patient is something I see a lot in my practice. This piece tries to explain what reactive hypoglycaemia is and give tips on how to manage it.
I’ll start with diagnosed reactive hypoglycaemia but I’ll also talk about people who seem to have large drops in blood glucose after they eat which they perceive to be associated with certain symptoms, like dizziness, light-headedness and more.
Post-prandial reactive hypoglycaemia
This is when you get low blood glucose following a meal or drink. The low can occur at any time in the post-prandial period but it’s normally from 2 to 4 hours after a person eats.
Understanding the cause of hypoglycaemia is really important, to make sure a person gets the right medical treatment where necessary, and the right dietary management as well.
Post-prandial reactive hypoglycaemia is perhaps best characterised and studied in people who experience it after having bariatric surgery, and these make up >95% of the patients with diagnosed reactive hypoglycaemia I see.
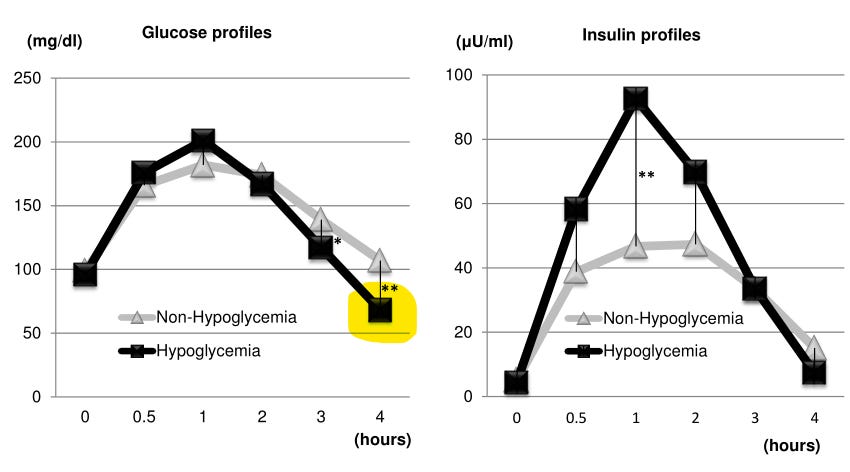
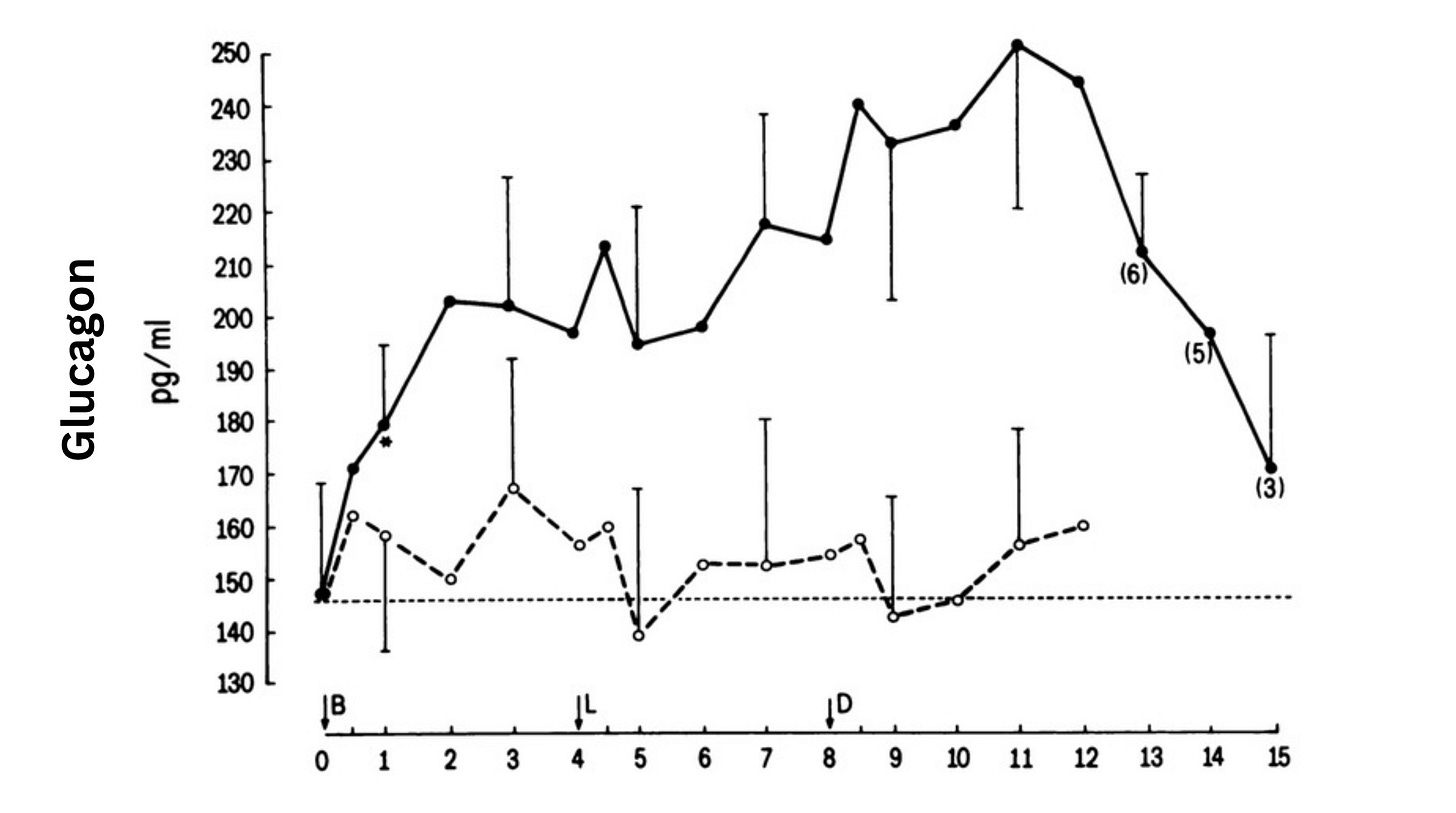
Based on physiological studies that examine whole body glucose homeostasis it looks like there is a mixture of increased insulin secretion, decreased insulin clearance and improved insulin sensitivity which is causing the hypoglycaemia. Additionally, people have defective counterregulatory hormone responses to hypoglycaemia. This means that the normal rise in glucagon which occurs when blood glucose gets too low - and which breaks down glycogen to produce glucose - doesn’t occur.
Dietary strategies
While we don’t have a lot of data on how to manage reactive hypoglycaemia we do have some.
High-protein, reduced-carbohydrate diets
Reducing the glycaemic load of the diet, by increasing protein and reducing carbohydrate seems to lower the glucose peak, and probably by doing so prevent some of the over-exaggerated insulin response.
However, just as important - and a unique characteristic of this diet - is that protein increases glucagon. So if there is still some exaggerated insulin response even with a reduced glycaemic-load diet, glucagon counteracts the effect of insulin on glycaemia - maintaining euglycaemia.
Low-carbohydrate, or low glycaemic index diets.
There is also some evidence that very-low-carbohydrate (aiming close to ketogenic) and low-glycaemic index diets can help prevent reactive hypoglycaemia, even without increasing protein much. The mechanism here seems to be that since the rise in glucose itself is much lower, and the rate of increase is slower, you don’t get as much of an exaggerated insulin response that then brings glucose crashing back down again.
For some patients, advice to lower the carbohydrate content of every meal - for example, under 25g of carbohydrate for main meals - works well.
Getting a greater proportion of carbohydrate from low-glycaemic carbohydrates is also an option. Lactose in dairy is very low-glycaemic, as is fructose - eg pop 1/2 mango in a salad (about 10-15g fructose). However, note that in some, too much fructose can cause gastrointestinal discomfort so may not be suitable for all.
Changing the food order - protein and vegetables first and then carbohydrate last can also be a strategy which is effective.
You might have read that cold pasta produces a smaller glucose excursion compared to fresh pasta. And that reheating cold pasta lowers glucose even further. This is true, and can be an additional strategy to enjoy your favourite pasta meals while reducing the risk of reactive hypoglycaemia.
Medications like acarbose - which work by reducing the digestion and absorption of dietary starch - also seem to help keep blood glucose levels more stable, prevent over-secretion of insulin, and prevent the large dip in blood glucose.
These are strategies I have seen used in my practice (acarbose prescribed and managed by endocrinologist) with success.
What about eating small frequent meals?:
I should just note that one of the things I’ve noticed occasionally is that sometimes patients that have reactive hypoglycaemia are encouraged to eat more frequently or even sip orange juice to “prevent hypos”. This doesn’t make sense with post-prandial reactive hypoglycaemia because it is disordered prandial metabolism which causes it.
So unless there is a particular reason why you need to eat smaller frequent meals, I would not recommend this. You’ll make your life easier by sticking with 3 meals a day (and a snack if you need), and eating in such a way that you do not trigger an exaggerated insulin response.
You feel like you’ve got reactive hypoglycaemia, but upon testing your glucose is normal
There’s a lot that we don’t know about the human body and when people seem to have normal clinical measures - or what we understand to be in the normal clinical range - it can be frustrating for patients.
It’s especially difficult when we’re dealing with symptoms like tiredness, lack of concentration or dizziness which are non-specific symptoms and they could have any number of causes.
I see quite a few of these kinds of patients in my practice, who seem to be having these symptoms about 2 to 4 hours after they eat, and while blood glucose looks a bit low on a CGM, or even upon standard medical testing, it’s still within the normal range.
I think in these cases it’s important to strike a balance between acknowledging what the patient is experiencing, while providing guidance and support which at the very least is not going to do harm and hopefully helps. It may well be that the body doesn’t just respond to the absolute concentration of glucose, but may also sense the steep gradient when dropping; and it’s this which is enough to trigger some symptoms.
So in these people, again I think the most appropriate advice is to limit the glucose peak and by doing so hopefully limit insulin secretion which should stabilise glucose.
Stage one advice for these people would be to have meals with a low-glycaemic carbohydrate, include plenty of veggies and healthy fats to slow down glucose absorption and of course include protein. This is healthy eating advice anyway, and if it helps improve symptoms, then great.
You could also try changing the food order again (eating the protein/veges first, before the carbohydrate) to see if it makes a difference.
Note that in rare conditions (neonatal diabetes), some people get an exaggerated insulin response to more protein, which itself can lead to hypoglycaemia.
What if you don’t get symptoms, but you’ve been wearing a CGM and you get a really low dip in glucose?
Here I would highlight that most CGMs are not particularly accurate in the hypoglycaemic range. Compression of the sensor (e.g. if a person lies down, or somehow squashes the CGM against the skin) can also give artificially low readings. It doesn’t mean they’re completely wrong, but sometimes noting their limitations can provide reassurance to people who think their blood glucose is getting dangerously low. A finger prick measure using a glucometer is a more accurate way of just checking, and as always, if you’re worried about something, check with a doctor.
Finally, a slightly high-ish fasting glucose, and a low 2-hour glucose can sometimes indicate “early” prediabetes. I’ll write about this more next week. Cheers.
Disclaimer
As a dietitian, and not a medical doctor, I am not qualified to diagnose any health conditions.







I am experiencing this but I’m in recovery from anorexia so it is very hard to follow restrictive advice when I’m meant to be upping my intake of everything. I make sure I always include fats and protein but still suffer - shivers, blurred vision, shakes. I’m not recovering from a super low weight, I wonder if the reactive hypoglycemia will right itself with consistent eating and healthy weight? I severely restricted carbs for years and reintroducing them has had an incredible benefit to my mood…Hard as GP not interested so am trying to navigate it on my own! Any suggestions who to go to for help?
Your posts have finally begun to shed some light on my symptoms. I’m not diabetic, I train 12-15 hours/week and I got a CGM bc my A1c is 5.7-6.2. My CGM shows I have pp hypoglycemia (and I FEEL it!!) as well as post exercise (and often during exercise) hypoglycemia. Eating more carbs before exercise makes it worse. Also dairy makes it worse. I’m already eating protein (100-120g/day) and 40-50g of fiber/day. I’ve been to 4 dieticians and 3 sports med doctors and no one has any advice. The only thing that helps is not training. 🤷♀️ there is something going on, but the usual low glycemic advice isn’t working as well. I look forward to more posts and hopefully I’ll be able to pull out a helpful thread.