My blood glucose got to 7.0mmol/L - is this diabetes?
The difference between a normal acute increase and standardised diagnostic cut-offs
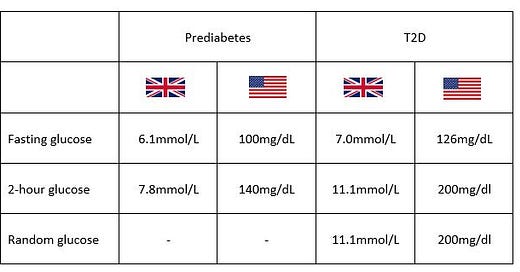
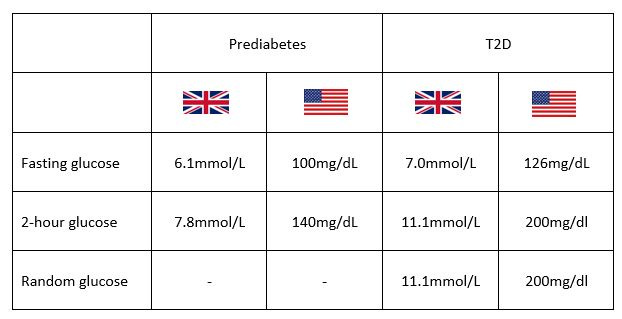
I previously described how T2D and prediabetes can be diagnosed based on a fasting glucose and a 2-hour glucose (and a random glucose for T2D only).
And I think because of this, people can easily freak out when they see a value of 7.0 (126mg/dL) or 7.8 (140mg/dL) or even 11.1 (120mg/dL) on their CGM devices. Like “oh people with diabetes have a glucose above 7, and this is bad, so I need to keep mine below 7 at all times”. Or “omg I just had a banana and my glucose is 7.8mmol/L - this is prediabetes”.
But there are important caveats to these numbers:
Acute versus Continuous
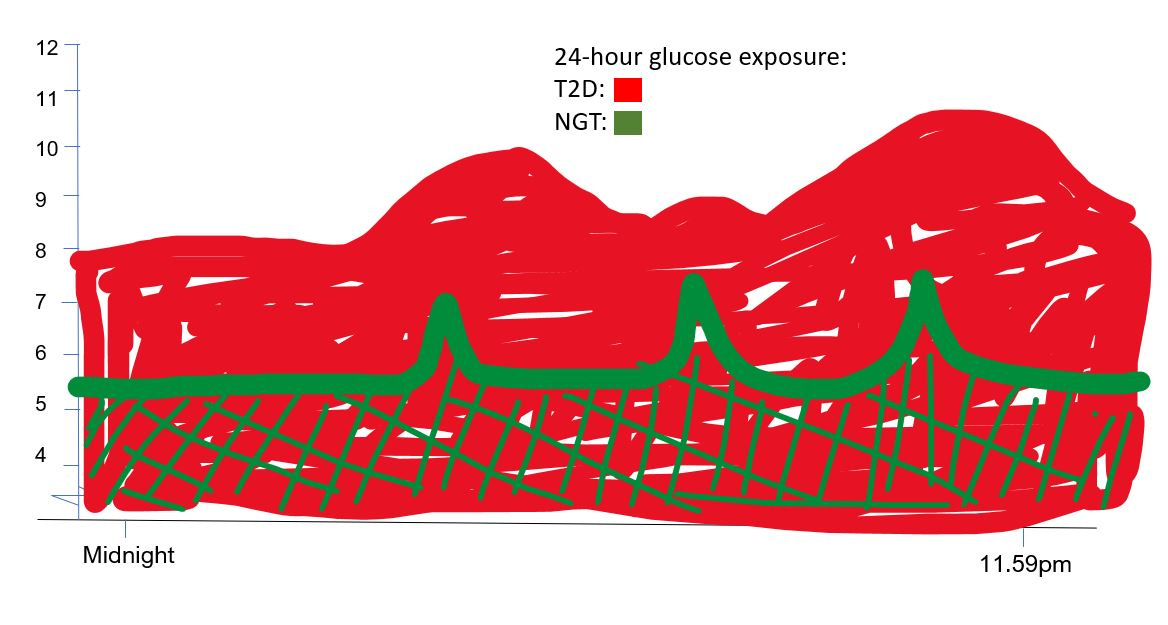
If someone’s fasting glucose is 7.0mmol/L (140mg/dL) or higher, this means that their glucose has probably been high most of the night (even taking into account the Dawn phenomenon).
And remember, a large part of the reason we have 7 as the fasting glucose cut-off in diabetes is because people with a fasting glucose of at least 7, almost always have a 2-hour glucose of 11.1 (200mg/dL) or more. This means that someone probably has a glucose which runs between 7 and at least 11 (140 and 200mg/dL) the majority of the time.
Compare this to your glucose reaching 7 (140mg/dL) for brief periods during the day. Not comparable.
Well, what about the 7.8mmol/L figure? Remember this tests measures blood glucose 2 hours after a glucose drink. It is completely normal for your blood glucose to go up this high 30 minutes after a drink of 75g glucose, but it is not normal for glucose to stay this high up to the 120 minute point. And if glucose is still at 7.8mmol/L at 120 minutes it’s an indication that 1) your beta-cells aren’t working properly, 2) you probably also have insulin resistance and 3) your glucose has been at least 7.8 for the better part of 90 mins. (And the underlying pathophysiology [which is causing the *symptom* of hyperglycaemia] could be a/the(?) predominant(?) cause of type 2 diabetes/CVD etc.
Compare this to your glucose going up to 7.8mmol/L for 15 mins and coming back down again. Not comparable.
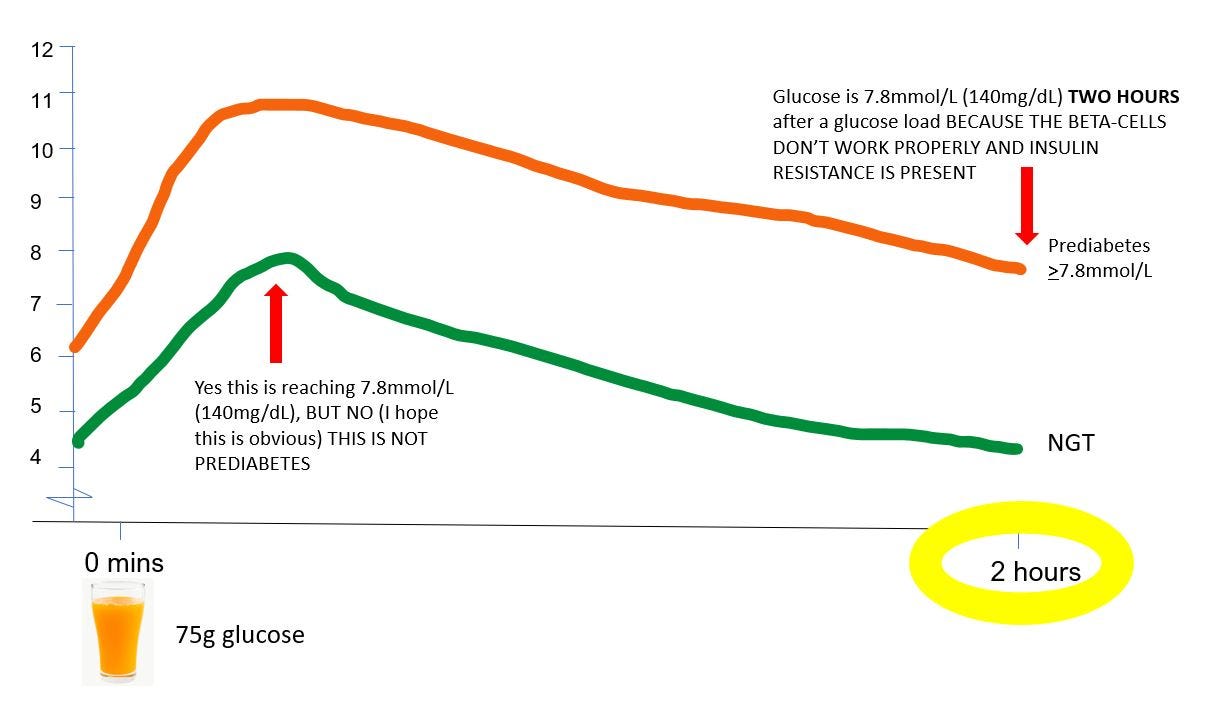
Well, what about the 11.1mmol/L figure? The same points as I made above stand with respect to glucose still being 11.1 two hours after a glucose load not being the same thing as glucose reaching 11.1 briefly and then coming down.
But - in healthy individuals, average peak glucose after an oral glucose tolerance test isn’t much above 7.8mmol/L (140mg/dL). Does this mean that if your blood glucose goes above 7.8 at any point - even acutely - this is bad? Not necessarily in my opinion.
It’s important to note that an OGTT is typically done in the morning, and oral glucose tolerance seems to be highest in the morning, especially in lean individuals. If an OGTT is carried out later in the day (and whether fasting is 8 or 12 hours - ie circadian rhythms are accounted for), glucose will run higher.
It’s also important to note that although a 75g glucose load is a lot, a pizza might have +100g, and so it would be reasonable to expect that glucose might go higher than 7.8mmol/L (140mg/dL).
But - does it matter if it goes up to +11.1mmol/L (200mg/dL) and then comes back down pretty quick? In other words, does having a high glucose for eg 15-20 minutes per se cause damage to cells and tissues, and meaningfully contribute to the development of serious diseases? To my knowledge, noone knows for sure, and I think most people would say this is where things get a bit unclear.

Here is my thinking:
It might be instructive to note that in this study people with a BMI of ~23kg/m2 with an HbA1c of 5.0% get peak CGM readings of 9.4mmol/L (171 mg/dl) after a standardised meal which had 50g of carbohydrate, and 9.3mmol/L (168mg/dL) for free choice meals which had up to 95g of carb per meal and varying amounts of protein. And it’s probably very likely that if these individuals are getting peak readings of around ~9.5 during this study, that they have them all the time, and still maintain an HbA1c of around 5.0%. And an HbA1c of 5.0% is not associated with CVD. So, getting sensor glucose readings up to 9.5mmol/L probably occurs in very healthy people, and is no reason for concern*.
In this study 7 out of 32 people, with mean BMI 25kg/m2 had period of at least 10 minutes where their glucose exceeded 11.1mmol/L (200mg/dL). The mean HbA1c of the group was 5.3 +/- 0.3% - the paper doesn’t say whether these 7 individuals who reported the highest CGM values had higher HbA1c. But nevertheless, it is not even clear that the risk of CVD goes up at HbA1c of 5.3%. So again, it’s probably possible to have short periods of time where glucose does in fact exceed 11.1mmol/L (200mg/dL), and maintain an HbA1c that is not associated with things like CVD.
So in summary:
In the absence of evidence to the contrary, I think it’s safe to say that CGM peaks of 9.5mmol/L are normal, and probably occur in a lot of metabolically healthy, lean people and probably are nothing to worry about*.
Peaks of around 11.1mmol/L probably? aren’t unusual. If you have a truck load of carb in one go, I don’t think it would be unsurprising to get a sensor reading this high, but maybe if you’re getting them a lot, it might be a sign you are developing some intolerance to glucose. But guess, what, you’ll probably also notice your HbA1c creeping up, maybe your waist circumference creeping up - and these are markers which have a lot more certainty with regard to any health risk.
And this second point here really leads on to “if I am getting high glucose readings on a CGM what I should I do?”.
If you’re thinking “AH BUT HBA1C DOESN’T CAPTURE PEAKS AND DIPS LIKE CGMS DO”, you’re correct. This is called glucose variability and I address it in this post.