You might have heard me talk a fair bit on recent podcasts about why I don’t think endurance athletes or high-volume exercisers should be worried that their high carbohydrate intake could be leading to type 2 diabetes (T2D).
I wanted to lay this out in a bit more depth in this post.
First of all, we know a lot about how T2D develops, and very, very little suggests that starchy carbohydrate intake causes it even in regular, non-high-volume exercisers. (Note, I am making an important distinction here between starchy carbs like potato, rice, and bread vs fructose/sucrose which we’ll touch on later).
What do we know about how type 2 diabetes develops:
The two primary pathophysiological causes are 1) defective insulin secretion and 2) insulin resistance across multiple tissues.
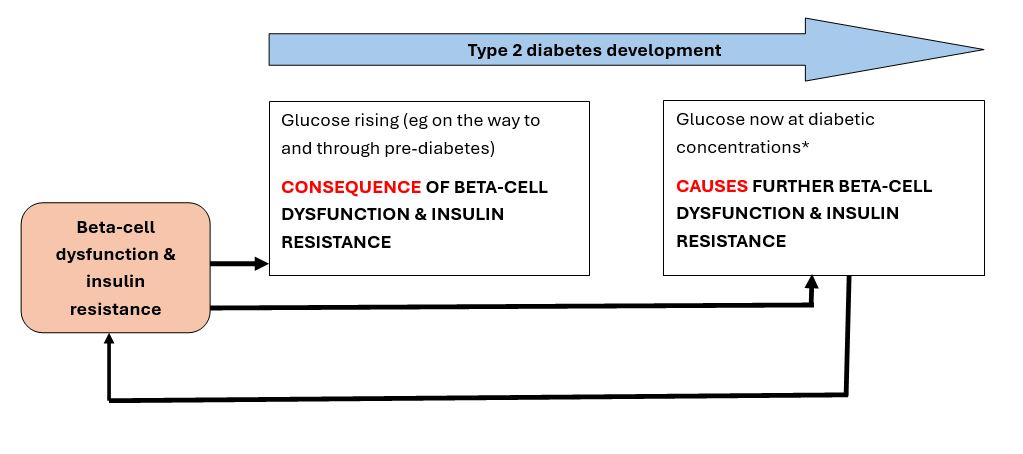
These pathophysiological defects are present BEFORE we see changes in glucose.
This gives us a very good idea that pathological defects cause glucose to go up, not that glucose going up causes pathological defects.

So what causes the pathophysiological defects in the first place? This is really hard to study and very complex but we think the following are the main ways:
An excess of calories in susceptible individuals (genetically or epigenetically susceptible) causes fat to be deposited as visceral or ectopic fat (basically fat being stored somewhere it is not normally stored), and somehow disrupts the function of organs like the pancreas, and liver.
Adipocytes (fat cells) secrete stuff like inflammatory and immune compounds which when chronically elevated, disrupt key metabolic organs and functions including the beta-cells and insulin signalling in the muscle.
Visceral fat may be particularly harmful in this regard, as this is the fat that surrounds our key organs (pancreas, liver etc). And anything secreted from intraperitoneal fat (a specific visceral fat depot) drains into the hepatic portal vein - in other words straight to into liver.
Sedentary lifestyles also promotes underlying pathophysiological changes that lead to the development of T2D, e.g. a short period of inactivity impairs hepatic glucose metabolism; and inactivity promotes fat deposition in the liver.
Genetics: normoglycaemic offspring of people with T2D have impaired beta-cell function.
Now there are other some smaller things which might also contribute:
If chronic inflammation disrupts organ function, then anything that causes chronic inflammation probably also does. The microbiome might be important here, and not having enough whole, fibrous foods plays a small role.
A low-fibre, refined diet with insufficient whole fruit and vegetables may also unfavourably alter body composition.
There is some evidence that replacing saturated with unsaturated fats could improve insulin signalling, but this effect is tiny compared to calorie excess and exercise.
Lots of liquid sucrose/fructose may also increase hepatic lipogenic activity and generally impair glucose and fat metabolism (and this becomes relevant when we’re taking about athletes).
Menopause seems to promotes fat deposition in unhealthy places.
So, it’s not carbohydrate then?
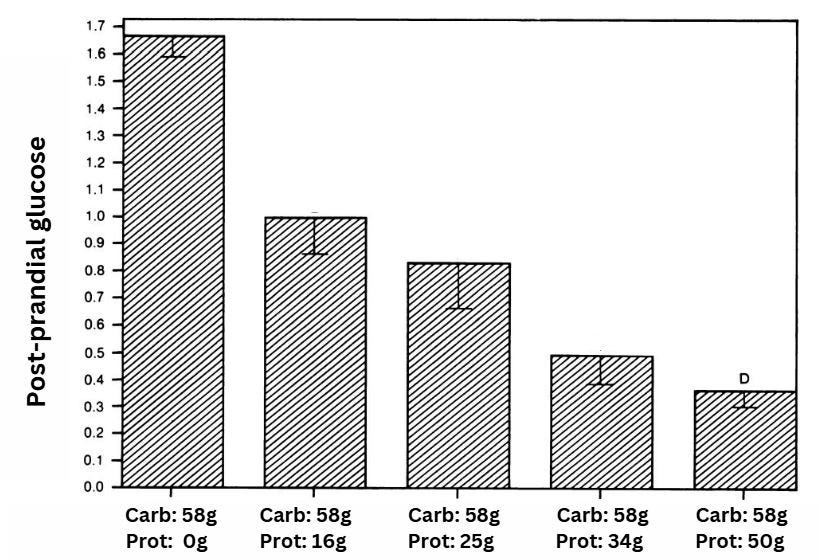
No, I really don’t think so. Not only do we have a lot of evidence about what causes T2D - and none of these pieces of evidence have anything to do with carb intake - we also have evidence showing modifying the amount of carbohydrate in the diet does very little to alter T2D risk. (Glycaemic index does, but it’s far more likely to be because low-GI carbohydrates are inherently high-fibre - hence it’s the fibre that is protective against T2D). Furthermore, dietary protein reduces post-prandial glucose in people without diabetes; and yet total protein is not protective against the development of T2D in any way we can measure.
This might be surprising to people who have heard that “glucose causes insulin to rise and this causes insulin resistance”. While prolonged hyperinsulinaemia (when insulin is elevated continually 24h a day) has been shown to harm beta-cell function and cause insulin resistance, moderate reduction in carbohydrate intake doesn’t have any significant effect on 24h insulin concentrations. Now it’s certainly true that going super low-carb (ie keto) does significantly lower glucose and fasting insulin, but what it also does is significantly increase 24h triglycerides and circulating free fatty acids (FFA). And what do elevated 24h triglycerides or FFA do? Cause insulin resistance HAHAHAHA*.

Are there glucose-infusion studies that show hyperglycaemia itself causes insulin resistance? Yes, but to my knowledge the “hyperglycaemia” achieved from the glucose infusions in these studies was the hyperglycaemia of diabetes - not moderate increases that we are talking about in normoglycaemia or even moderate prediabetes. It is widely known and acknowledged that once glucose gets to a certain concentration and stays there for hours and days (basically the concentration you see in diabetes) then it becomes a cause of subsequent pathology but at the present time, all evidence suggests that on the way to T2D, the elevated glucose is a symptom of underlying pathology. Make sense?
Bottom line
Nothing I can see suggests lowering glucose per se is protective against T2D, and - to reiterate - this is because T2D is caused by beta-cell dysfunction and insulin resistance - which themselves cause glucose to go up. And even if it did(!), limiting carbohydrate doesn’t even affect glucose levels because the body adapts to it…..unless you cut carbohydrate low enough to be ketogenic……… at which point the reduction in circulating glucose is replaced by an increase in circulating fat…….which itself causes insulin resistance.
So, yeah, taking everything together, we know a lot about causes of T2D and none have to do with excess carbs or moderate rises in glucose alone. Simply put: causally, it’s more accurate to think of T2D as a disorder of fat metabolism than as a disorder of glucose metabolism.
But, but, endurance athletes consume a SHIT-LOAD of carbohydrate - surely they are a different case?
Ok, let’s look at this. Yes athletes, do consume loads of carbs compared to average people, but they also oxidise a ton of it. And remember, T2D is caused by chronic fuel surfeit, lack of physical activity, excess visceral and ectopic fat depots, and chronic inflammation. Most endurance athletes may struggle with consuming sufficient calories; and they don’t need to worry about a sedentary lifestyle as a risk! For the others: exercise protects against ectopic fat deposition, even without weight loss, and probably lowers inflammatory markers (but certainly doesn’t seem to increase them).
So exercisers (not just endurance athletes) are really protected from the typical pathophysiological pathways that underlie T2D so far as we know.

Fructose
Now, one potential risk I have seen highlighted is that of fructose. Most carbs we consume are from starches. These are chains of glucose that we metabolise in a well-regulated manner in the sense that our bodies can adjust to increases/decreases in starch quite easily by up/down-regulating enzymes and such. Unless we overconsume calories or the diet is low in fibre/inadequate nutritionally, high-starch intakes don’t lead to impaired fat or glucose metabolism so far as we know**. Fructose though is different.
Fructose has distinct metabolism compared to glucose; and if too much is consumed, evidence in humans suggest it can lead to impaired fat and glucose metabolism. Let me be clear here that there is a ton of fear-mongering about fructose which is unwarranted - the harm seen in trials is only (to my knowledge) when fructose is given in high amounts, and in liquid form. So yeah, basically sugar sweetened beverages.
So how much is enough to “overload” us?
Liquid fructose intake of 80g/day has been shown to cause dodgy changes in fat metabolism in regular, healthy people. For context, mountain dew is about 75g fructose per litre. A lucozade energy gel (45g packet) has about 10g fructose.
Athletes may come close to or exceed 80g/day. In fact, since intestinal absorption of glucose is a primary limiting factor of exogenous glucose availability, and ingestion of glucose with fructose increases absorption (because they use different transporters in the intestine), many endurance athletes will intentionally aim to get high proportion of their carbohydrate from fructose.
So does the high consumption of fructose in athletes cause the same metabolic derangements as it seems to in less active controls? It doesn’t seem to, and happily it seems that athletes are particularly good at using fructose as an energy source. For example, at the extreme end, endurance athletes are able to consume close to a gram of fructose (0.8g) per minute over 120 minutes, but are able to convert most of the fructose to glucose and lactate which are subsequently oxidised. But reassuringly, even more modest types of activity seem to favourably alter the way fructose is metabolised, or at the very least prevent the detrimental changes in fat metabolism that can be induced by excessive fructose. In a very cool and elegantly designed study Luc Tappy and team showed that in calorie excess(!) and with 30% of calories from fructose(!), pretty modest physical activity (30 mins cycling twice a day at 120W), prevented the metabolic dysfunction that occurred in the control group who were not exercising.
Can athletes basically eat what they want then?
This is where I think things get interesting and there’s a tiny bit of nuance to this. In general we have to acknowledge that T2D is primarily caused by visceral and ectopic adiposity, inactivity, with a bit of genetics thrown in.
But there are other dietary risk factors which could be playing a role - albeit a much tinier role - the greatest of which is probably that of fibre and whole plant foods.
I think having a "healthy” microbiome is pretty important for how we metabolise energy, and there is some clinical data, with more come showing that fibre/whole food intake seems to modulate body composition. Furthermore, the microbiome is linked to stuff like whole body inflammation, so I think it’s smart to look after it as much as possible. Could there be a risk that athletes are so focused on calories, carbohydrate and protein that they might not prioritise fruits and vegetables and stuff? Maybe.
So if athletes are concerned about their risk of T2D, my advice would be to try to get as many whole plant foods and fibre in as possible. Obviously this can be challenging because vegetables can fill you up without providing much energy or starchy (available) carbohydrate. But consider foods like nuts, seeds, and avocado. Even adding a tablespoon of legumes to large(!) plate of rice is a good idea. And when you’re having vegetables, be super generous with the fat (frying in rapeseed oil or adding a large drizzle of olive/walnut/avocado oil to them) to keep calorie intake high.
Caveats
Most of the above is talking about the development of T2D in people who are currently healthy and pretty lean. It is fair to acknowledge that things do get more grey with regard to the effect of carbohydrates on insulin resistance etc in people who already have overweight/obesity or already have some insulin resistance or metabolic syndrome. In general, exercise is such a potent beneficial modulator of metabolism that I think the effect of high-carbohydrate/fructose intake would be negligible, but it’s fair to acknowledge we don’t have good data on this.
*If you read around this area a lot, you might be thinking, but high carb diets also increase triglycerides don’t they? They do, but in healthy people only fasting triglycerides increase on a high-carb diet; post-prandial TGs are lower. And a general theme throughout metabolic research is that it is the chronic elevation of things like glucose, inflammatory factors, insulin, FFA and TGs that is the problem.
** There is a question about how much this is true for people who are already overweight and or have insulin resistance/metabolic syndrome. Gerald Reaven has written thoughtfully about this, but to be clear here I am not talking about carbohydrate intake in people who already have metabolic syndrome or are not exercising.
Disclaimer
As a dietitian, and not a medical doctor, I am not qualified to diagnose any health conditions.









Fascinating, thanks. What about carbohydrate restriction as a treatment for people who already have T2D? The Guardian gave a relatively favourable review to Gary Taubes' recent book which made the argument that diabetes treatment has not been sufficiently focused on carb restriction, but Taubes's previous books have not been well-received by nutrition scientists:
https://www.theguardian.com/society/2024/jan/14/unlocking-the-truth-about-diabetes-is-it-time-for-a-diet-based-treatment
This is great 👍